
I love teaching classes about sex at senior living communities. It’s a great way to validate and honor our elders’ humanity, their need for connection, and search for intimacy. Yet almost every time I teach, I get questions about residents expressing themselves sexually in ways that are unwanted or challenging. Dementia and lack of awareness are often challenging for senior living administrators and staff. Think about these difficult situations and consider what you might do.
1. If loving you is wrong
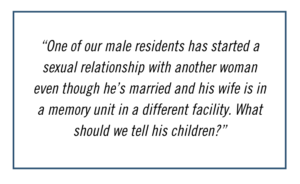
Sometimes older adults express their sexual desires to someone other than the person they’re married to and it causes discomfort to others. Have you ever had to deal with a situation where:
- a cognitively impaired spouse begins to show a sexual interest in someone other than their partner?
- the partner of a cognitively impaired person finds a new relationship without telling their spouse?
- both partners with cognitive impairment express their sexual desires in public?
When dealing with cognitive impairment and sexuality, it is important to have frank discussions with the spouse and family members. It is also important to talk with the person who is the new object of affection (as well as their family members) to get more clarity on each of their concerns. It could help to have an outside expert mediate these kinds of discussions.
2. Bringing the #MeToo Movement to senior living
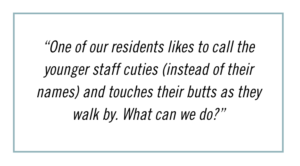
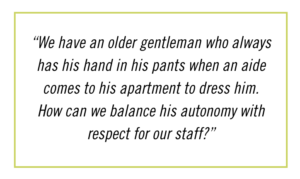
The #MeToo movement has shed light on sexual harassment, defined as any unwanted sexual attention, verbal or physical sexual advances, requests for sexual favors, and other harassment of a sexual nature. How we handle residents who may be unaware of the #MeToo movement or sexual harassment laws can be difficult. Have you ever been faced with:
- a “handsy” resident who can’t stop touching the staff?
- an upset staff member who walked in on a resident touching themselves?
- a resident who requests extensive genital care from certain staff
Your role as a clinical or administrative leader is vital to setting the policies and training for residents as well as staff. Trying to balance the realities of sexual expression while fostering an environment of safety and health for staff and other residents can be difficult to handle. You might need outside help to create a safer and healthier work and living environment.
3. Handling dilemmas gracefully
We often need help finding more resources before beginning to tackle these and other difficult situations. Training materials need to be made available for staff to help balance autonomy and safety. Policies need to be crafted for consistency. But how do we talk about these concerns gracefully? Handling dilemmas like these can lead to uncomfortable situations with family members as well as staff. Not only the adult children — but other friends and relatives — may be distressed. Family members and staff rarely think of elders as sexual beings. Along with your problem-solving strategies, you can remind them gracefully that sexuality is a fundamental part of our humanity, no matter how old we are.
4. Sexual expression and cognitive function
Lindau and her colleagues (2018), in a national study of over 3000 adults with a mean age of 72, found that nearly 50% of all men and 18% of all women with dementia were sexually active. Among older adults with an intimate partner, 59% of men and 51% of women with dementia were sexually active. Among those 80-91 years old with an intimate partner, more than 40% living with dementia were sexually active. More than one in 10 people living with a partner reported feeling threatened or frightened by a partner. These people all lived at home. We can change that scenario in senior living communities by creating environments balancing pleasure with safety.
5. Creating an environment balancing pleasure with safety

As an administrative or clinical leader, you must create an environment that is safe for all while focusing on residents’ quality of life. Specifically focusing on sexuality can be daunting in this context. Begin by reviewing your policies and procedures regarding your organizational values, consent, privacy, family concerns, assessment of cognitive and physical abilities, staff development plans, and training. Consider each resident’s medical and sexual history, involve the family for help in providing relevant information. Ozkan and colleagues (2008) studied the use of behavioral and/or pharmacological therapy for inappropriate sexual behaviors. Plan strategies in advance to help decrease or minimize discomfort, insist on non-judgmental attitudes, use humor carefully, conduct staff training, and consult best practices throughout the industry.
As a staff member, remember to set clear boundaries with safety first, maintain a non-judgmental attitude, use humor carefully, consider alternatives to inappropriate touch, and discuss any uncomfortable situations with your supervisor.
6. Assessing abilities to consent
No single assessment tool yet exists to establish sexual consent when cognitive function has been impaired. Yet these tools can be a start. Using a mini-mental state assessment can give us an immediate sense of the resident’s ability to consent and we can continue the evaluation. Scoring below a certain threshold might mean the resident is unable to consent. Other variables to assess are the resident’s ability to avoid exploitation, awareness of the relationship, and awareness of risk. Consider the resident competent to participate in an intimate relationship only if they are able to avoid exploitation, aware of the relationship, and aware of risk. While no overall tool to establish consent exists, there is a pressing need for one to be developed.
7. Need for an overall understanding of the issue.
Inappropriate sexual behavior is an area of special concern. I’ve covered cognitive impairment and lack of knowledge here. It may be something completely different in your community. These understandings are part of a whole new area of sexuality and aging in senior living communities. We need sexual wellness policies, better assessment tools, clearer understandings of boundaries, and so much more. These can only begin when we start conversations, obtain more clarity, and incorporate sexuality into our organizational values and mission around safety, health, and wellness. Your leadership can directly improve the overall health and well-being of an elder in your community. They are depending on you.
There is no expiration date on sex. If your interest has been sparked and you have questions about this topic or you’d like more information on other topics related to sex and aging, it’s not too late to ask. Please write to Dr. Fleishman at jane@janefleishman.com. All emails are confidential and she will answer your question directly.
References
Ozkan, B., Wilkins, K., Muralee, S. & Tampi, R. (2008). Pharmacotherapy for Inappropriate Sexual Behaviors in Dementia: A Systematic Review of the Literature. American Journal Alzheimers Disease and Other Dementia, May. https://doi.org/10.1177/1533317508318369
Lindau, S. T., Dale, W., Feldmeth, G., Gavrilova, N., Langa, K. M., Makelarski, J. A., & Wroblewski, K. (2018). Sexuality and cognitive status: A U.S. nationally representative study of home-dwelling older adults. Journal of the American Geriatrics Society, 9, 1-9. https://doi.org/10.1111/jgs.15511


 Dr. Jane Fleishman
Dr. Jane Fleishman